What Nurse Anne taught me about diabetes in schools

Meet Nurse Anne
She’s the district nurse at Springfield Unified, a district of 8,814 K-12 kids across 14 schools. Her real name is Anne Johnson, but to everyone at school she’s just Nurse Anne: every day, she goes above and beyond to ensure the health and safety of all her kids and staff. If you’ve been at a school in her district in the last 15 years, chances are you’ve been helped by Nurse Anne.
- To Her Kiddos: Nurse Anne is tough yet fair. Serious, yet the first person you want around when something goes wrong. It breaks her heart to see these kids — young, innocent kids, living with serious chronic diseases they’ll battle for the rest of their lives. But her kids wouldn’t know it. She believes in building their independence — independence in managing their disease that lets them live their life to its fullest.
- To Her Staff: She is a trusted professional that has helped handle some really tricky health situations. She has time for less and less of the hands-on care she perfected as a pediatric nurse of 15 years and mom of 2 teenage boys, so she does her best to impart her knowledge on her staff.
- To Her Administrators: She’s a fierce advocate for health in schools. She’s not afraid to go to bat for what she believes in, even if it means disagreeing with the people signing her paychecks.
- To Parents: She’s a trusted caregiver that does a lot for their kids, though they wish she had more time to dedicate to taking care of them personally. She wishes she did, too…
How I met “Nurse Anne”
Nurse Anne’s story is one I heard over and over as I was meeting with school nurses from school districts all over California. The purpose of these interviews was to understand how health is managed in schools— and, more specifically, how diabetes is managed in schools.
I started this project hoping to apply my experiences from living with and building products for diabetes toward improving the way diabetes and other health issues are managed. I was diagnosed as an adult and as a result I could make my own decisions about how to live my life. Kids don’t have this luxury — they rely on their parents, family, and, when they go to school, school staff like Nurse Anne to keep them safe and healthy.
So I met with school nurses to understand a day in their life with managing diabetes — 57 school nurses to be exact. Together, they represent:
- 25 school districts
- 287,000 students
- 330 kids with diabetes
Here’s how the interviews break down:

What I learned from Nurse Anne
School nurses care about what they do — a lot. They are extremely knowledgeable and experienced, and if there were a Nurse Anne in every school, this project could have been pretty boring. But there’s not. Not even close: in CA schools, there‘s ONE nurse to every 2,582 kids. The numbers for California schools are jaw-dropping:
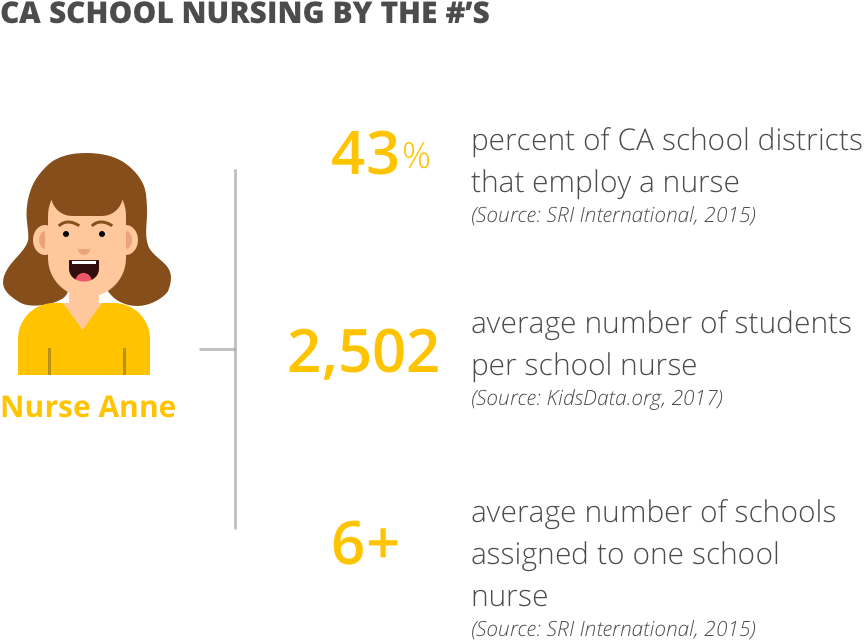
Nationally, these numbers are a little better, but still not great:
74.8% districts employ a nurse (with only 39% full-time)
1,691 students per school nurse
(Source: National Association of School Nurses)
If kids were only dealing with bumps and bruises, stomach aches, and sore throats, these numbers might make sense. But they’re not. Kids today suffer from major-league health issues — issues like diabetes, asthma, and severe allergies that require dedicated care from trained staff.
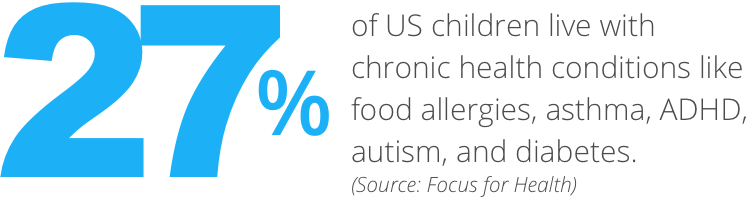
So what do schools do? As I learned, they make do with what they’ve got: they train whoever is available. This usually means training unlicensed staff like office secretaries, teachers, or health aides.
Why this is a Problem
Challenge #1: Managing chronic conditions is really hard (especially when you’re a kid)
For kids with diabetes, tight glucose management is essential to short- and long-term health. This translates to estimating food, delivering insulin for meals and high glucose, and eating carbs. Each of these takes time and requires significant decision-making skills to perform effectively.
Now imagine you’re a child with diabetes in school. You haven’t developed the physical or mental skills needed to manage a chronic condition, so you rely on Nurse Anne and trained school staff to make your diabetes decisions. Here’s what a morning might look like:
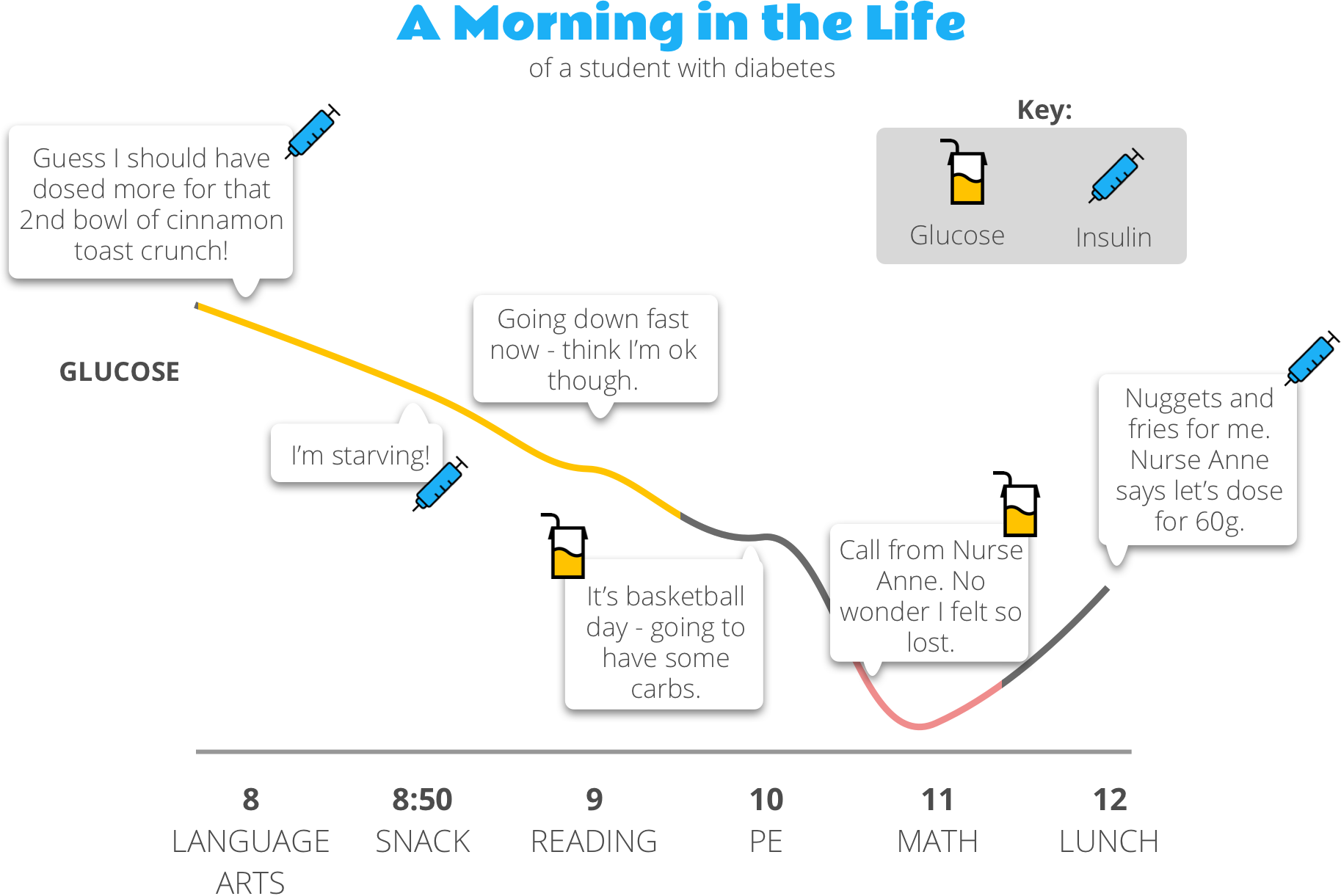
If this looks complicated, well, that’s because it is. Glucose is affected by everything — food, stress, hormones, exercise…add to it being a kid in a busy school day getting care from school staff, and well, things get quite a bit tricker.
Challenge #2: Health resources at schools are limited.
Health isn’t a priority in schools unless it becomes an immediate issue.
I heard this over and over from nurses I spoke to.
We’re spread so thin — we do the best with what we have.
If we had another kid diagnosed with diabetes, I don’t know what we’d do.
You have to change your strategy so you can deal with it, but it becomes a problem when you have multiple schools, multiple students, and convoluted doctor’s notes. It’s not helping us, it’s making us have sleepless nights.
(Public) schools are legally responsible for providing sufficient accommodations to children with disabilities under Section 504 of the Rehabilitation Act of 1973. Chronic diseases like diabetes are covered under this statute, meaning that schools must take steps to remove barriers that would otherwise limit the child’s access to the general education curriculum.
How the school accommodates the child depends on the state, the school, and the family, and there is significant gray area in how care is delivered. I heard a number of considerations that factored into resourcing for diabetes 504 plans, including:
- Age/independence level of the student: Students in elementary school are significantly more dependent on staff than those in middle school and high school, and schools are more willing to allocate dedicated resources to ensuring their care. Usually this translates to having a nurse come to the school at lunch — either one employed by the district or one contracted on a part-time basis.
- Availability of existing resources: Sometimes schools get “lucky” — and trained staff are already available at the school location — e.g., through an existing IEP/504 plan or a staff member has a child with diabetes.
- District Policies: Some districts are just more accommodating than others. They see the challenge of delivering care to kids with diabetes and take steps to secure resources. Many I spoke with followed a plan where only licensed staff can give insulin — often this is more of an informal guideline than a rule, but one that makes acquiring dedicated nursing staff more clear-cut.
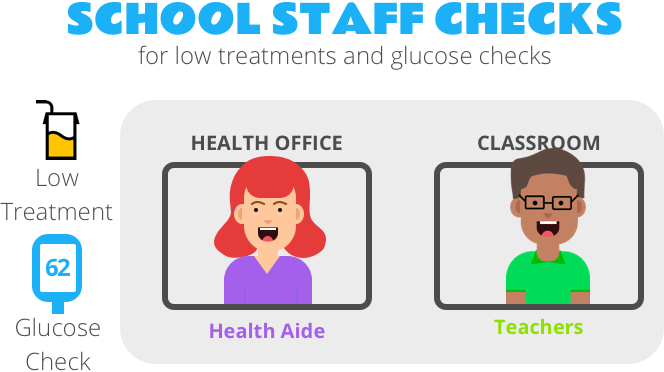
When it comes to resourcing, EVERY school, regardless of the above considerations, trains unlicensed staff to provide basic emergency care management, primarily for low glucose situations. These are the staff that are closest to the student throughout the school day and can be there to intervene if necessary.

Schools differ when it comes to the staff that deliver insulin. The most common scenario I found was a mix of licensed and unlicensed staff, where licensed staff are available for “scheduled checks” (e.g., times like lunch where insulin is given at the same time every day) and trained, unlicensed staff are available for the rest of the school day. Still, these models varied across districts, and I saw examples where only unlicensed health aides or only licensed health aides deliver insulin.
Challenge #3: The process of a school managing care is complicated.
For schools, the process for providing care to a student with diabetes is quite involved. Here’s the general process the nurse/staff follows when handling diabetes at school:
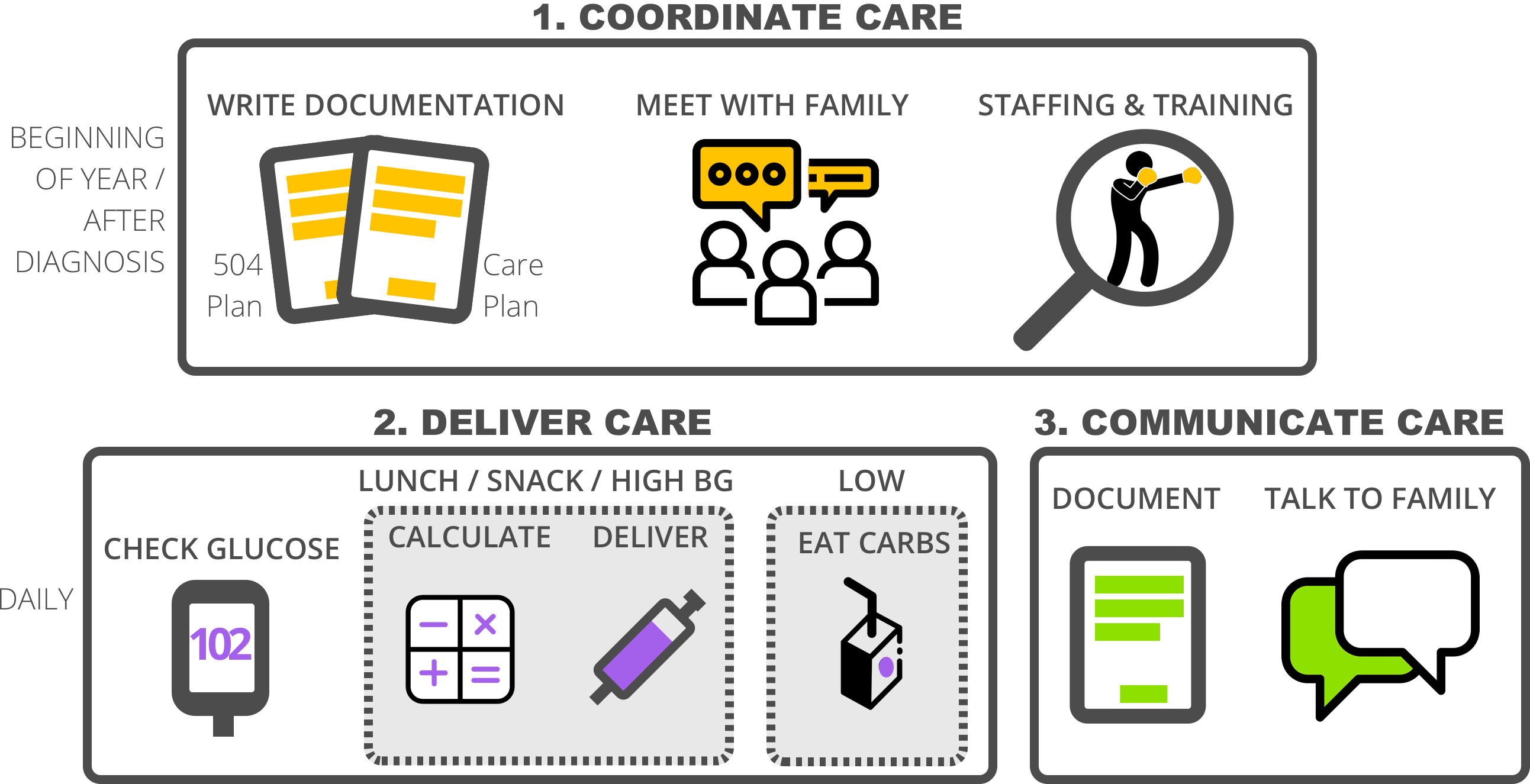
Coordinating Care:
- 504 Plan and Care Plan: When a student is diagnosed with diabetes — or at the beginning of the school year for an existing diagnosis— the school nurse coordinates how care will be delivered. Official accommodations are documented in the 504 plan and specific, individualized care instructions are documented as part of the Health Plan.
- Meet with Family: The family, administration, teachers, and any health staff meet to agree on the plan to keep the kid safe at school and that sufficient steps are taken to accommodate their care.
- Staffing & Training: Staffing needs are defined and training is carried out, usually by the school nurse (when there is one). This usually takes the form of the school nurse spending lots of time with the staff member(s) — especially the one(s) giving insulin. For teachers, it’s usually more of a heads up on how to manage lows in the classroom.
Delivering Care:
- Scheduled checks are usually planned so that insulin can be delivered for food (e.g., like for lunch and snack-time). In the schools I interviewed, this is usually a “roving” procedure nurse (Registered Nurse or Licensed Vocational Nurse) that visits multiple schools so they can give insulin to the children.
- Unscheduled checks are for when things don’t go exactly according to plan (i.e., every day with diabetes). This usually falls on the teachers and health aides. Managing lows are the most common — and biggest concern for staff.
Communicating Care:
- Logging interactions is something every school nurse does. Manually logging the BG, insulin administered, and any notes about the interaction. Mostly this is for liability or reference purposes.
- Talking to the family is another (usually) daily activity. In the most extreme examples, parents have asked to be notified before giving any insulin; in the most common case, parents are notified for any low or high treatments via phone call or text. In the best circumstances, staff members at the school and family members become trusted partners to best support the child.
Challenge #4: School nurses have a lot on their plate!
To top it all off, nurses have a lot of other things they manage daily. This article would exceed the word limit if I had to write at length about the full responsibilities of a school nurse, so here’s an overly simplified version instead:

Now What?
I’d love to make health a priority in schools, increase the number of licensed staff like Nurse Anne, or better yet, reverse the growing number of health issues kids face today. But these are huge challenges and we have to start somewhere.
So I’m starting with training and education:
- We need to fundamentally change the way we approach learning about a disease. Yes, diabetes and other health issues are complex, but they don’t have to be so hard to learn.
- We need to make better use of the resources that exist today in schools. Well-trained staff will translate to better daily care for kids with chronic health issues and ultimately, better long-term outcomes.
- Managing a kid’s health issue is a team sport. Let’s embrace this and better empower school staff, parents, kids, and healthcare providers.
- School nurses spend a significant amount of time being the advocates and trainers for health issues. It’s time they have access to tools that make their lives easier so they can focus on broader school health issues.
Finally, thank you to all you school nurses and health aides who go above and beyond every day to ensure the health and safety of your kids. Our families and schools are lucky to have you.
