Monitoring Blood Sugar

Monitoring Blood Glucose
Finding Balance
The first few years after I was diagnosed with type 1 diabetes, I absolutely hated checking my blood sugar. I’d be out with my friends or in class, and I’d have to pull out this old-school looking black case, take out a test strip, insert it into a product that looked like it was made in the ’80s, poke my finger to get some blood, and put the blood on a tiny strip…all to get a result I didn’t want to see.
It drove me to check less and less — until eventually, I was only checking once or twice a day.
The problem? Our blood sugar is constantly changing with life, and so only having this information only once or twice a day was just not enough. (It eventually led me to missing a really high blood sugar for 2 straight days during finals and needing to get hospitalized.)
Eventually, I learned the hard way that knowing my blood sugar level took away a bunch of stress and fear. Rather than worrying if I was going to go low or finding out too late that I had a high blood sugar, I could just get the information I needed and fix it before anything bad happened.
No…I still don’t love monitoring my blood sugar — I’d happily hand the job back to my pancreas if I could. But it’s also taught me a lot — including discipline and how my body works — so in the end, I’d say it’s all been worth it.
Here’s what monitoring blood sugar is all about.
Fun Fact: “Blood Sugar” and “Blood Glucose” are two different ways to say the same thing: how much sugar is in your blood. Glucose comes from the Greek word for “sweet.” It’s a type of sugar you get from foods you eat, and your body uses it for energy.
Balance Blood Sugar
When you live with diabetes, balancing blood sugar is the aim of the game.
- Too much sugar is known as a “high blood sugar”.
- Too little sugar is known as a “low blood sugar”.
The key is getting just the right amount of sugar — not too high, and not too low.

In the short-term, keeping a balanced blood sugar keeps you feeling good and avoiding interruptions to your day. Long-term, it keeps you healthy.
How Balancing Blood Sugar Works
Blood sugar is exactly what it sounds like — how much sugar is in your blood. Balancing blood sugar is maintaining that “just right amount of sugar” level.
For people without diabetes, this process is auto-magic:
- The body is constantly monitoring blood sugar.
- If it starts getting high — like after you eat a meal — it releases insulin to bring it back down. This helps sugar get from the blood to the cells to be used as energy. This lowers blood sugar.
- If it starts getting low — like if you’re exercising — the body releases something called glucagon to trigger more sugar to be made and released into your blood. This raises blood sugar.
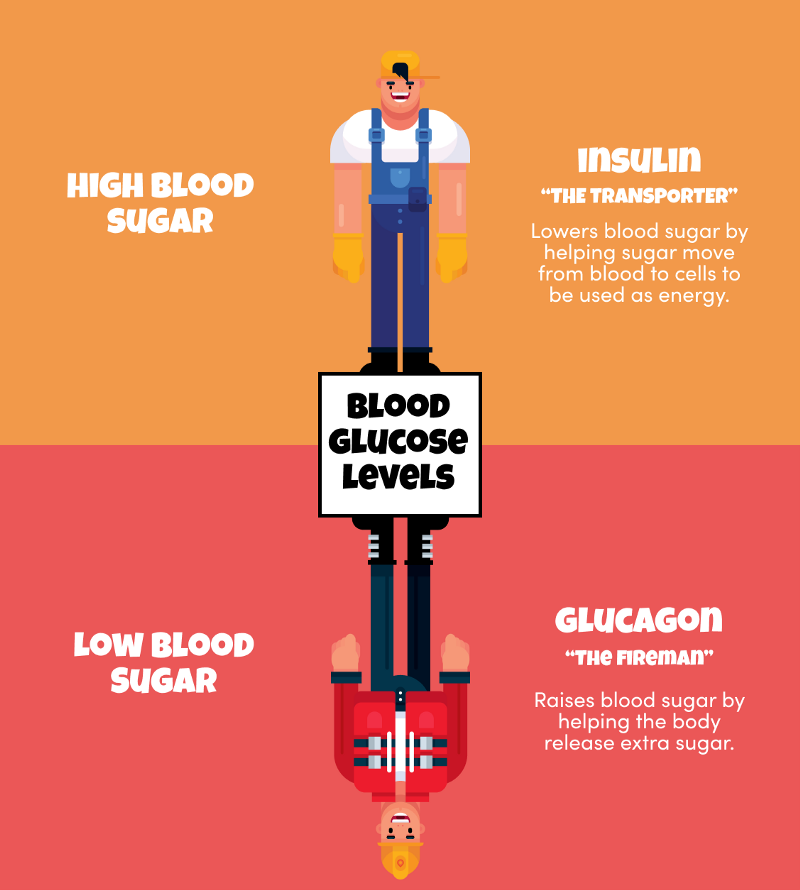
This process works over and over throughout the day to keep blood sugar balanced.
But when you’re diagnosed with diabetes, this process stops working. For people with type 1 diabetes, the body stops making insulin and glucagon like it should, leaving you to play the role your body used to do for you.
Here’s what you’ll need to do.
Monitoring
When you monitor your blood sugar, you’re checking how much sugar you have in your blood.
There are 2 ways to do this:
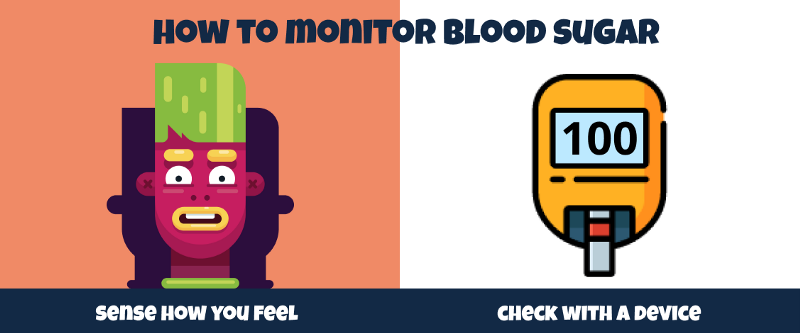
1 — Monitoring How You Feel
Your body will give you signs when your blood sugar is low or high:
- For a low blood sugar, this includes feeling dizzy, shaky, and hungry.
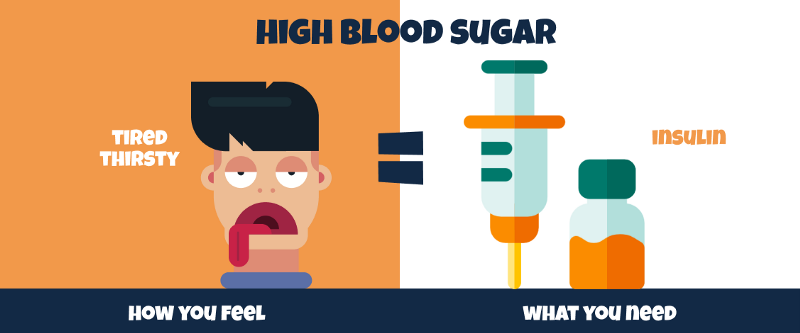
- For a high blood sugar, this includes being thirsty, tired, and peeing more than usual.
Because everyone will feel their lows and highs slightly differently, it’s a good idea to figure out how you personally feel for each so you quickly detect when your blood sugar is low or high and take the right steps to bring it back in range.
2 — Checking with a Blood Glucose Meter or Continuous Glucose Monitor
The best way to get the exact info you need is to manually check your blood sugar level. There are two types of devices that provide glucose information:
- A blood glucose meter: This involves poking your finger to get a small drop of blood and using a test strip to measure how much sugar there is in it.
- With a continuous glucose monitor (or C-G-M), you wear a small sensor on your body and it estimates how much sugar there is in your blood 24x7.

For both methods, you’ll see a number that represents how much sugar is in your blood.
When In Doubt — Do Both
While both approaches are good, the best approach is a combination of sensing how you feel and checking your blood sugar with a device. It can be easy to miss or confuse signs of a low or high blood sugar and doing both will help you avoid emergency situations.
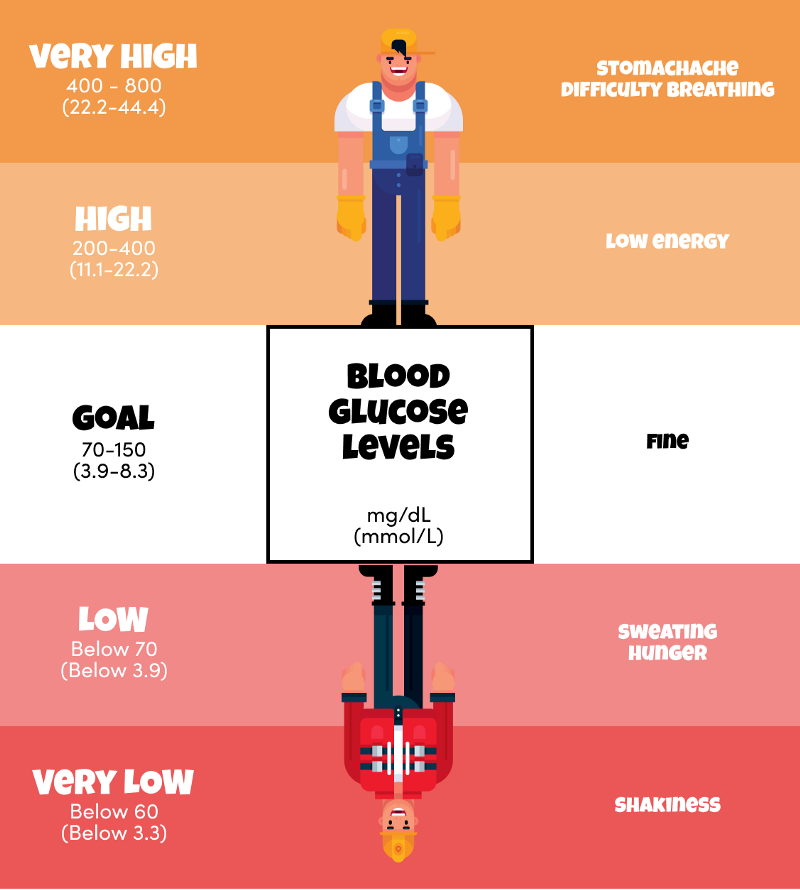
Blood Glucose Goals / Targets
The goal or target range for your blood sugar is generally 70–150 mg/dL. Below this range is a low blood sugar and above this range is a high blood sugar.
Fun Fact: mg/dL is the standard glucose measurement in the US, France, Japan, Israel, and India. mmol/l are used in Canada, Australia and China. Germany is the only country where medical professionals routinely operate in both units of measure. To convert mmol/l to mg/dl, multiply by 18.
Low Glucose (Below 70 mg/dL | 3.3 mmol/L)
Imagine being chased by a bear…how would you feel?

Probably:
- Shaky
- Lightheaded
- Sweaty
These are all the symptoms of having a low blood sugar.
So what can do you do about it?
Luckily there’s a pretty easy fix: eat some sugar. In this case, you want something that will get into your body really quickly. Fast-acting sugars are what you need — things like skittles or juice are perfect for the job.

Fun fact: Anything with carbs eventually breaks down into sugar. But some work faster than others, which is why you want “fast-acting-carbs” like juice and candy instead of “slow-acting carbs” like bread (which take too long to break down into sugar).
High Glucose (Above 200 mg/dL | 11.1–11.2 mmol/L)
You know that feeling when you’ve just eaten a really big meal and you start to get sleepy and tired?
This is a bit what it’s like to have a high blood sugar. The symptoms include:
- Feeling Thirsty
- Feeling Tired
- Peeing more than normal
- Feeling really thirsty
What you can do about it
Your body needs insulin. This will help the sugar in the blood get the cells to be used as energy.
Fun Fact: You might feel thirsty and pee more than normal when your blood sugar is high. This happens because the body is trying to flush out the extra sugar in your body.
Achieving Balance
Especially in the beginning, checking blood sugar can be a really demoralizing activity: it takes time, it hurts, and often the result isn’t what you expect. But over time, you’ll start to learn how your body reacts to food, activity, and stress, and you’ll learn what to do about it.
Figuring out how many times to check — and when — is a key to balancing your blood sugar. But don’t forget another important thing to balance — diabetes and your life.
Always make sure to check in with yourself and how you’re feeling. It can be easy for the result to feel like a test, but it’s not. A blood sugar result is just information that helps you figure out what to do. So try not to be so hard on yourself, give yourself space to learn, and you’ll be just fine.
And always remember: