Types of Insulin

Types of Insulin
The goal of managing type 1 diabetes is to control blood sugar — meaning how much sugar is in our bloodstream.
- Too little sugar (low blood sugar) can leave you feeling dizzy, shaky, and hungry. Even without diabetes, people feel this— maybe you did a bunch of activity and didn’t have any food. For people with type 1 diabetes though, this can be especially dangerous, because the body can’t recover from a low blood sugar the same way someone without diabetes can.
- Too much sugar (high blood sugar) can leave you feeling tired, thirsty, and peeing a lot. If left unmanaged, this can get serious quickly, leading to complications.
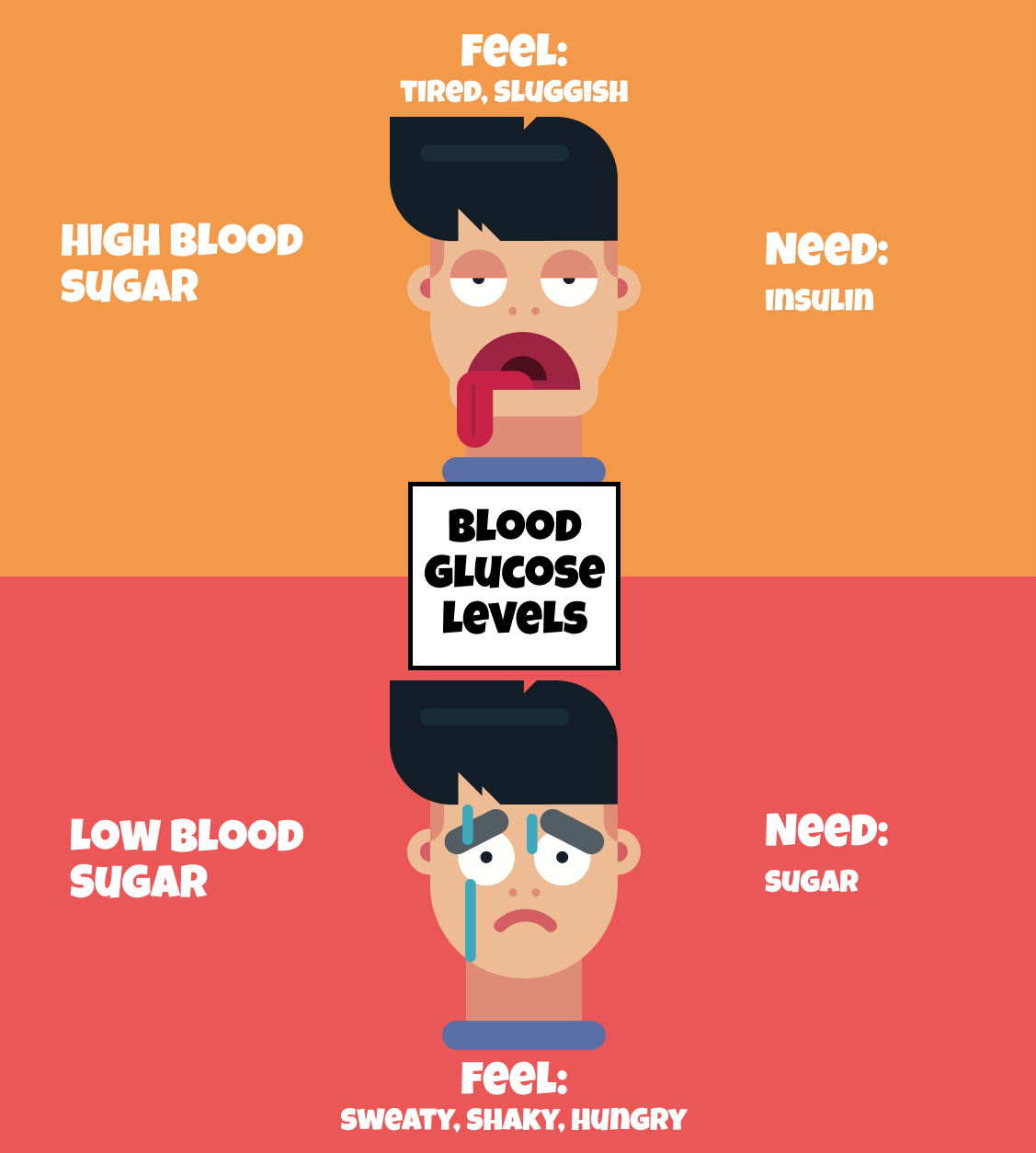
Too little sugar is fixed with eating some extra sugar (like some candy).
But what about high blood sugar? In this case, the body needs a way to get rid of some of this sugar.
That’s where Insulin comes in.
Fun Fact: Until the early 20th century, the only way to treat type 1 diabetes was with a strict low-carbohydrate, low-calorie diet. In 1921, Canadian surgeon Frederick Banting and his assistant Charles Best discovered insulin. The introduction of insulin as a treatment changed the outlook for people with this disease.
How Insulin Works
For people without diabetes, the process for balancing blood sugar with insulin is pretty smooth. As sugar enters our blood, the body makes some insulin, which helps the sugar pass into cells to be burned for energy.

But for people with type 1 diabetes, this process isn’t so smooth. Since the body isn’t making insulin, sugar builds up in the blood. This does 2 things:
- Blood sugar goes up.
- Our cells lack the energy they need.
Luckily there’s a fix: insulin. Insulin is injected into the body so the body can continue this process of moving sugar into cells to be burned for energy — the same way it would if it was making insulin naturally.
Easy, peasy, right?!
Wrong. It turns out our bodies are really good at balancing blood sugar levels…that is, when they’re working properly. But take away the ability to make insulin (as is the case for people with type 1 diabetes), and you’re putting a human in control of a process that used to work 24x7.
Instead, people with type 1 have to constantly monitor blood sugar and take insulin or sugar to balance out. To make things a little easier, new injectable insulins have been developed to help mimic what the body does naturally.
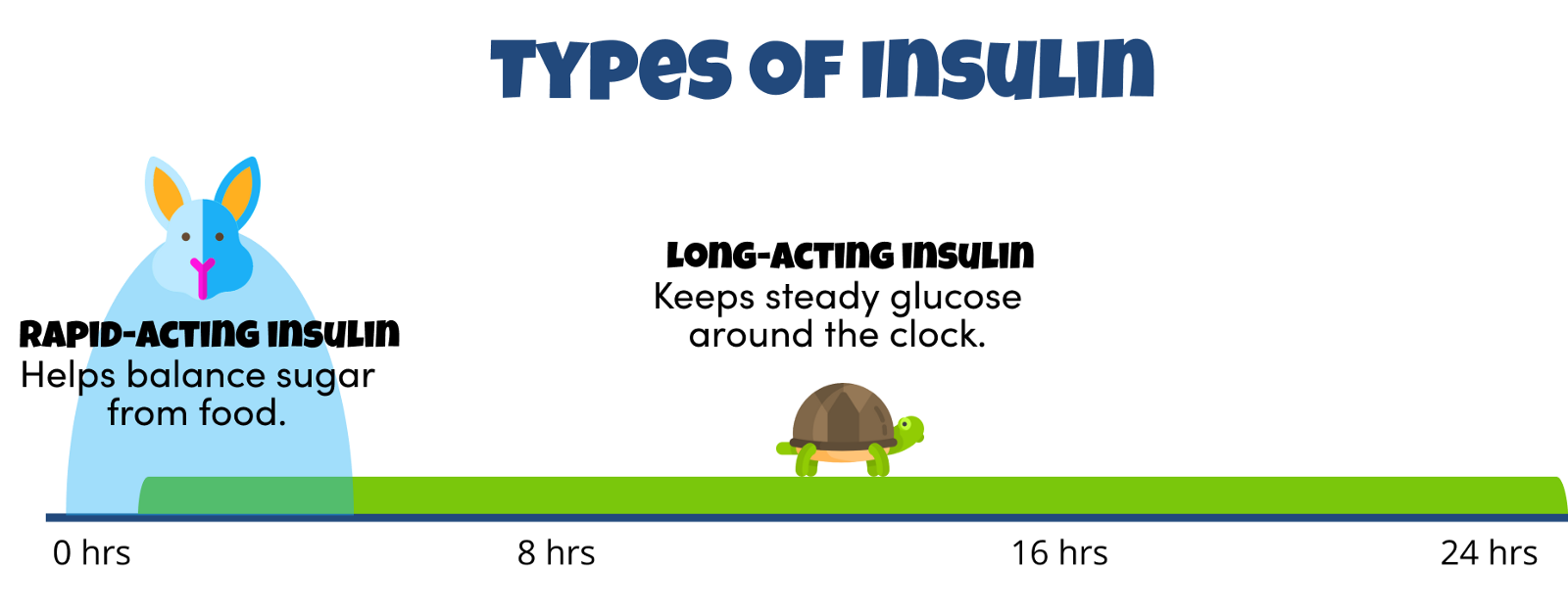
They’re called rapid-acting insulin and long-acting insulin.
Fun Fact: There is a 3rd type of insulin called “NPH Insulin” (aka regular insulin) that we won’t cover here. It’s generally considered less flexible than the more modern “analog” insulins that most people with type 1 use today due to how it peaks and how long it lasts in the body.
Rapid-Acting Insulin
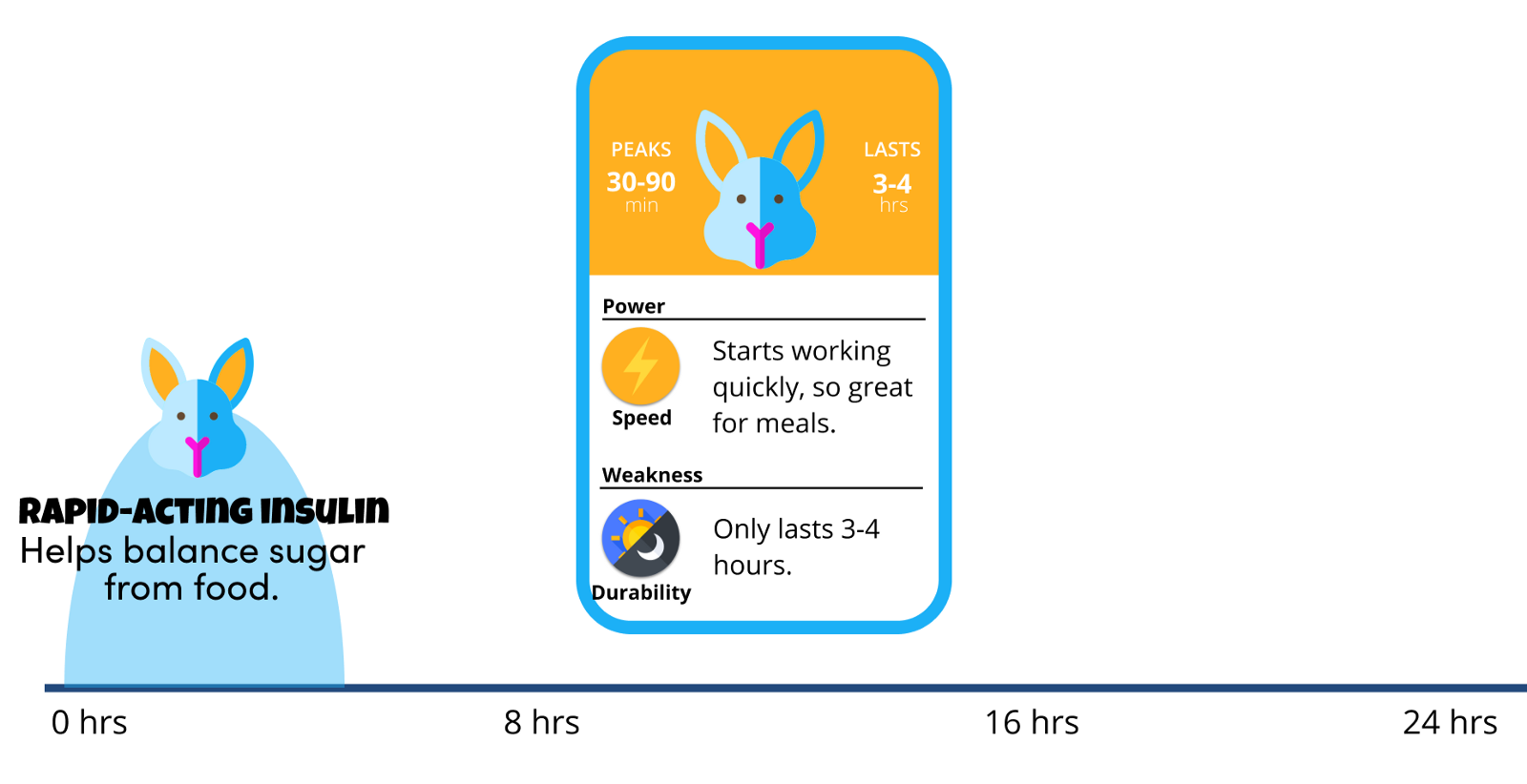
Rapid-acting insulin is used for 2 things:
- To stop the rise of blood sugar from eating food. As a result, most people take a shot of rapid-acting insulin before mealtimes.
- To “correct” a blood sugar that is too high.
Rapid-acting insulin begins to work about 15 minutes after injection, peaks in about one or two hours after injection, and last between two to four hours.
- The Good News: Works quickly, so great for meals.
- The Bad News: Only lasts 3–4 hours, so not a good option for stabilizing glucose throughout the day.
There are 4 main brands of rapid-acting insulin: Novolog (Novo Nordisk), Humalog (Eli Lilly), Apidra (Sanofi), and Fiasp (Novo Nordisk).
Long-Acting Insulin
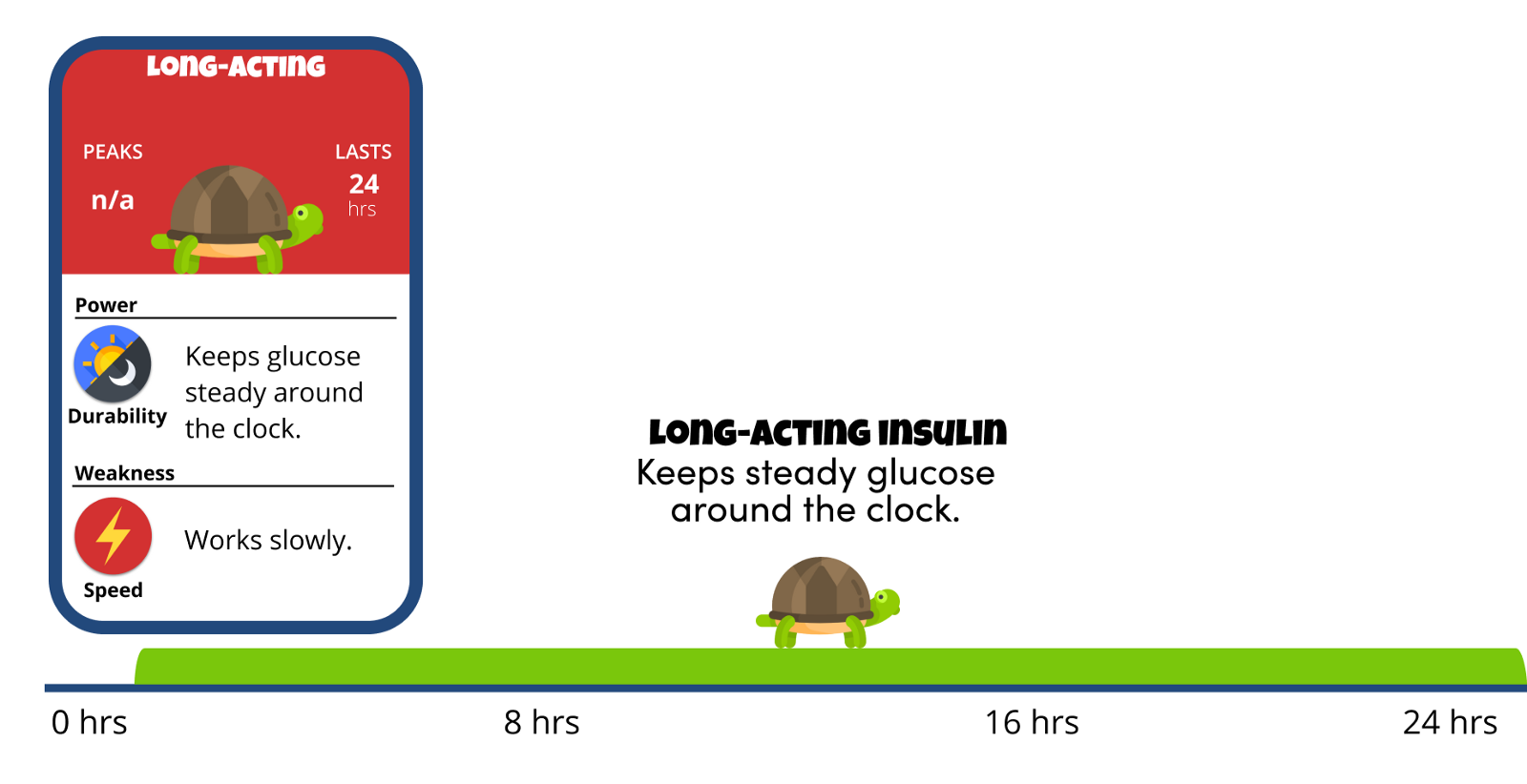
Long-acting insulin reaches the bloodstream several hours after injection and tends to lower glucose levels up to 24 hours.
- The Good News: Keeps glucose steady around the clock by giving your body a small, steady amount throughout the day.
- The Bad News: Works slowly, so it’s not effective with food.
It’s usually taken once per day to help prevent the liver from producing sugar and ketones and releasing them into the blood. For people with type 1 diabetes, it’s usually paired with rapid-acting insulin.
There are 5 brands of long-acting insulins: Tresiba (Novo Nordisk), Basaglar (Eli Lilly), Lantus (Sanofi), Toujeo (Sanofi), and Levemir (Novo Nordisk).
Fun Fact: You may hear Long-Acting Insulin called “Background” or “Basal” Insulin. Your pancreas normally makes set amounts of insulin around the clock. Basal insulin mimics that process, and your body absorbs it slowly and uses it throughout the day.
Delivering Rapid-Acting and Long-Acting Insulin
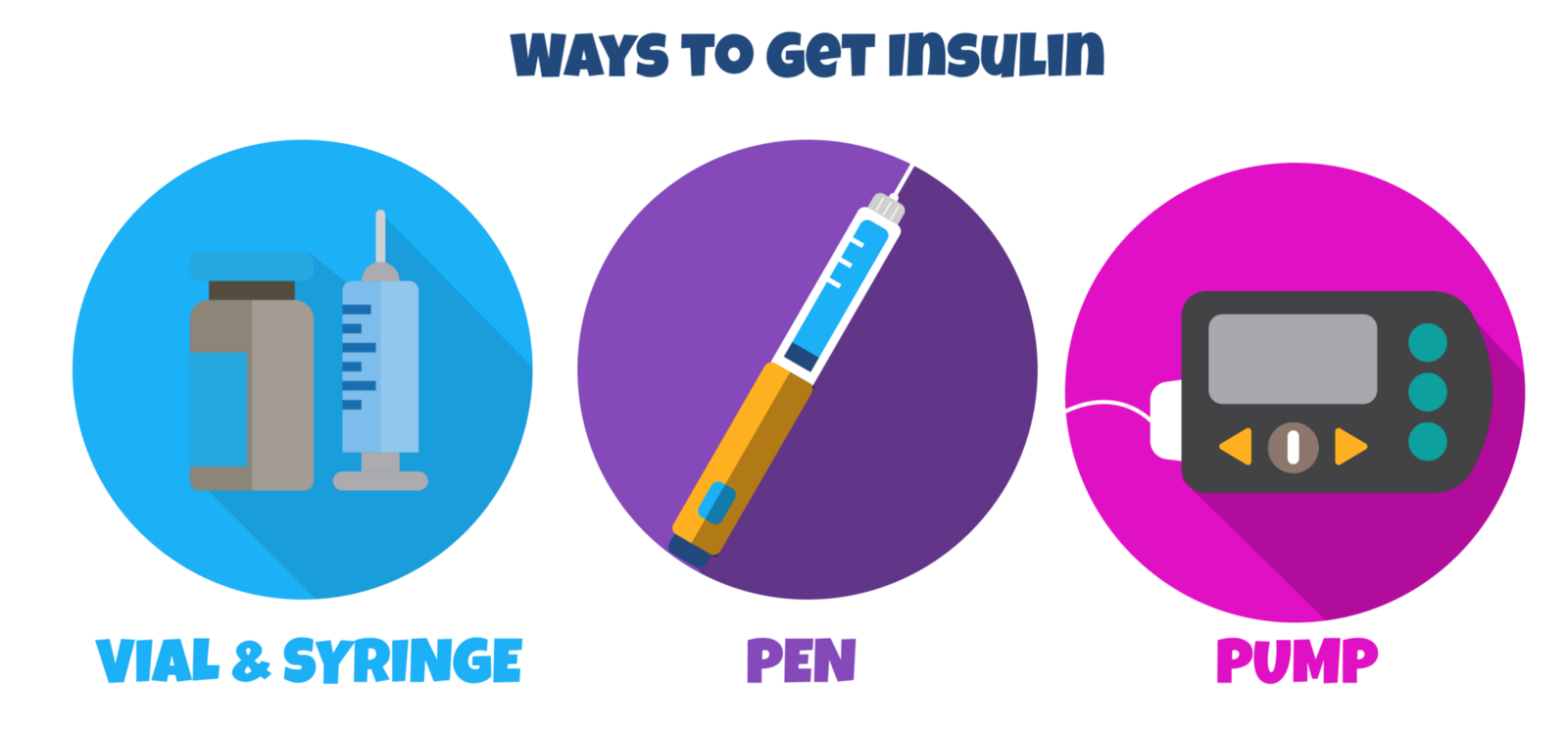
There are 3 ways to get insulin:
- Vial & Syringe: The insulin is stored in a vial and the syringe is used to inject.
- Pen: Insulin is stored in a pre-filled insulin pen and a small, replaceable needle is attached to the end to give the injection.
- Pump: Stays attached to your body and gives both continuous amounts of insulin throughout the day and insulin for meals.
Almost everyone starts with either a vial & syringe or insulin pens when they are first diagnosed.
Do Your Best, Forget the Rest
Hopefully you learned a little something about the types of insulin, how they work in the body, and what they’re used for. Just like glucose monitoring, it’s important to remember that this isn’t easy. The body is constantly changing with activity, stress, and food, and it’s constant work to keep up.
Insulin is your tool to help manage blood sugar, but it’s never perfect. Do your best to learn the basics, give yourself space to learn, and reach out for help when you need it. I’ve lived with type 1 for 15 years and I’m still learning. Just stick with it.
Do your best and forget the rest.
Practice Your Skills
Let’s see how we did — test your skills here!
